Nothing is hidden. If you look carefully, you will find all you need to find. In the study of newly diagnosed Scottish patients with MS, close to 40% had hidden disabilities such as depression, anxiety, fatigue, sleep disturbance, cognitive impairment and pain. Are these MS-related problems really hidden? Yes, hidden from the eye but detectable by simply asking the right questions and assessing the function of the nervous system using standard techniques.
A remarkable 26% of subjects were on antidepressants, 18% were unemployed, 36% had motor difficulties, 36% had balance, incoordination, double vision or swallowing problems and 12% had bladder or bowel problems at symptom onset.
These observations are not new and have been well documented in other studies. This study confirms that early MS is not really early MS, and a large proportion of pwMS have evidence of the damaging effects of untreated inflammation on the function of the nervous system.
In the majority of these subjects, the hidden symptoms remained unchanged, but in approximately a quarter, the symptoms improved after the diagnostic period. DMTs had no major influence on the hidden disability burden over a period of about one year. However, subjects treated with fingolimod and cladribine, higher efficacy DMTs, had a more favourable outcome. Is this not an argument for flipping the pyramid and using high-efficacy DMTs first-line in more pwMS? Is it not time to leave the less effective platform therapies as a historical footnote? In this cohort, over 1 in 5 patients were started on injectables (interferon-beta or glatiramer acetate).
What is quite remarkable is that this study represents 45% of the newly diagnosed people with MS in Scotland over the study period, with an average time between symptom onset and diagnosis of 18 months. This is a problem. If early inflammation imprints on the brain and spinal cord, waiting 18 months to be diagnosed and then a further period of time to be started on treatment comes at a cost. Unfortunately, the latter information is not reported in the paper. I am aware from other studies in the UK that the time from diagnosis to initiating DMTs is variable and can take anything from 2 months to 9 months depending on the kind of service the patients attend, i.e. a specialist centre versus a district general hospital requiring patients to then be referred to a specialist centre for treatment.
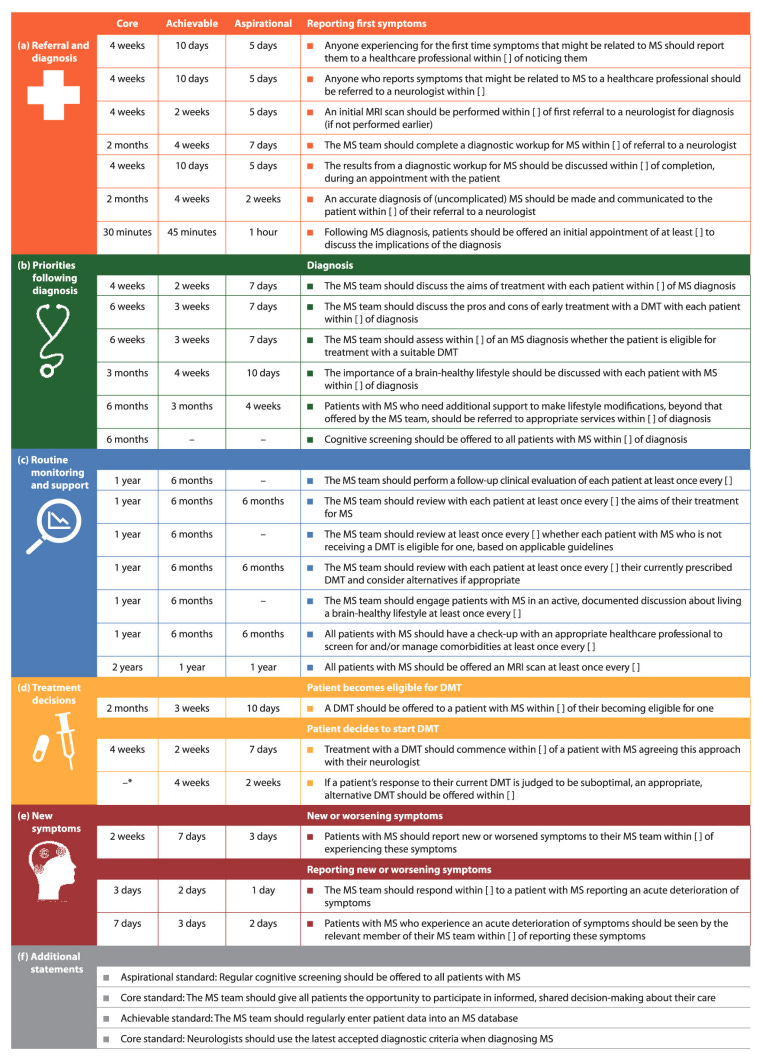
These delays due to systemic problems in the NHS cost our patients’ brain and spinal cord. These delays are the main reason we produced the ‘Brain Health: Time Matters’ policy document and the follow-on quality standards (see paper 2 below) to try and create the carrot and stick to sort out the unnecessary and unacceptable delays in the diagnosis and management of pwMS.
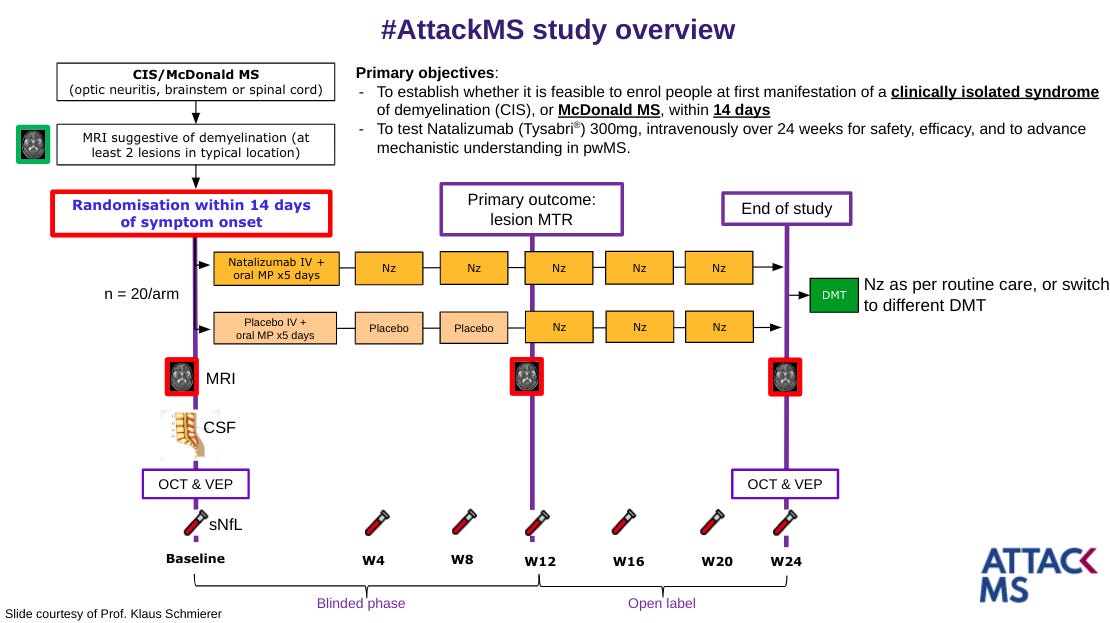
We are even taking this ‘Time Matters’ approach to the extreme with our #AttackMS trial, in which we are comparing pwMS started on natalizumab within 2 weeks of symptom onset to those starting natalizumab after 2 months. Yes, we really think time matters in MS; this study will tell us if weeks matter.
In our International Quality standards, which were developed by international consensus, we state the diagnosis of MS should be made within 2 months and a DMT treatment offered within a similar timeframe. Please note these are just the core standards, and we challenge the MS community to do better than this.
Sadly the NHS fails on these metrics, and the costs to pwMS in the UK is likely to be substantial. What can we do about it? We need more resources and a more responsive system to deal with MS. This can be done. The NHS has proven that if there is a will, there is a way to achieve things. It has been done for the management of stroke and, to some extent, with the two-week pathway for suspected cancer. Why can’t we get a 2x2 month pathway for the diagnosis and treatment of MS? Is this too little to expect from our national health service?
Paper 1
Glasmacher et al. The influence of disease-modifying therapy on hidden disability burden in people with newly diagnosed relapsing-remitting multiple sclerosis. Mult Scler Relat Disord. 2022 Apr 30;63:103837.
Background: In addition to motor disability, "hidden disability" such as depression, anxiety, fatigue, sleep disturbance, cognitive impairment and pain is a major complaint of people with multiple sclerosis. We explored changes in hidden disability burden in the early post-diagnostic period and examined the hypothesis that disease modifying therapies have a beneficial effect on hidden disability burden.
Methods: Adults with recently diagnosed (< 6 months) relapsing-remitting multiple sclerosis (n = 440, mean age 37.4 ± 10.4, 76% female), from a national multicentre cohort study (FutureMS) underwent testing with clinical and neuropsychological instruments as well as brain MRI at baseline and after 12-months. Disease modifying therapies were only started after baseline assessment and were classified into injectables (n = 70, interferons, glatiramer acetate), other DMTs (n = 215) and no DMT (n = 117, reference). Sensitivity analyses were undertaken using alternative classifications (disease modifying therapy vs none, and a 3-category system). We performed latent transition analysis with hidden disability burden as the latent variable including propensity score weights.
Results: We identified three classes with low (58%), moderate (25%) and high (17%) hidden disability burden. 70% did not transition ("unchanged", reference), 26% transitioned into a lower burden class ("improvement") and 4% transitioned into a higher burden class ("worsening"). Median treatment duration was 11 months (IQR 9-12). Injectables [OR 1.3 (95%CIs 0.7, 2.3); P = 0.4] and other DMTs [OR 1.4 (95%CIs 0.9, 2.1); P = 0.2] were not associated with significant change in hidden disability burden in either direction ("improvement" or "worsening"). In the alternative 3-category classification, category 2 treatment (fingolimod, cladribine, n = 22) was associated with improvement [OR 4.3 (2.6, 7.0); P < 0.001].
Conclusion: Hidden disability was present in most newly diagnosed people with multiple sclerosis. The majority remained unchanged and approximately a quarter improved over the immediate post-diagnostic period. Disease modifying therapy had no significant influence on hidden disability burden in the study period of one year following diagnosis. The trend towards favourable outcomes with fingolimod and cladribine should be interpreted with caution due to the small sample size. Our exploratory data are observational, with scope for attendant biases, but highlight the need for further study including longer-term evaluation as well as randomised trials for non-motor disability.
Paper 2
Hobart et al. International consensus on quality standards for brain health-focused care in multiple sclerosis. Mult Scler. 2019 Nov;25(13):1809-1818.
Background: Time matters in multiple sclerosis (MS). Irreversible neural damage and cell loss occur from disease onset. The MS community has endorsed a management strategy of prompt diagnosis, timely intervention and regular proactive monitoring of treatment effectiveness and disease activity to improve outcomes in people with MS.
Objectives: We sought to develop internationally applicable quality standards for timely, brain health-focused MS care.
Methods: A panel of MS specialist neurologists participated in an iterative, online, modified Delphi process to define 'core', 'achievable' and 'aspirational' time frames reflecting minimum, good and high care standards, respectively. A multidisciplinary Reviewing Group (MS nurses, people with MS, allied healthcare professionals) provided insights ensuring recommendations reflected perspectives from multiple stakeholders.
Results: Twenty-one MS neurologists from 19 countries reached consensus on most core (25/27), achievable (25/27) and aspirational (22/27) time frames at the end of five rounds. Agreed standards cover six aspects of the care pathway: symptom onset, referral and diagnosis, treatment decisions, lifestyle, disease monitoring and managing new symptoms.
Conclusion: These quality standards for core, achievable and aspirational care provide MS teams with a three-level framework for service evaluation, benchmarking and improvement. They have the potential to produce a profound change in the care of people with MS.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite that is currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription, to please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry or Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional who will be able to help you.
















I wonder if this sort of objective is easier to achieve in different health settings, where funding is better, or patients have only got access to healthcare through insurance. The NHS is in crisis really, so it may seem to be a pipe dream. My NHS trust is a sort of centre of excellence but since I re-registered to it having tried somewhere closer to home, I have not seen a neurologist. I am now down to a phone call a year. I am one of the least affected people I know, but nonetheless , this is pretty sketchy monitoring. I have the nous to get an MRI when I want it or to make contact with an MS nurse and I self manange with good lifestyle choices. Nonetheless with BVL and smouldering disease a worry, I don't feel very optimistic. I really believe that the big push you (et al) are making with Attack MS must be pushing policy in the right direction, but with the NHS and NICE currently as they are, it's an example of "the wheels grinding exceeding slow." Frustrating for HCPs and patients alike.
I was diagnosed in the US, I went to a doctor, then an opthomologist (presenting with optic neuritis) within 24 hours, then to the hospital and was given an MRI and diagnosed with MS within a day. I saw an MS specialist two weeks later and started treatment within 3 weeks of diagnosis (copaxone, was only offered that or interferon). Coming to the UK it took me 7 months to get seen and that would have been the delay also for continuing treatment even though I was on a first line, except I threw a big stink about it and was able to get the medication before that 7 months. I was told though, "if you decline then we'll see you faster and give you treatment" as if the treatment would turn back time and turn back brain damage. Without me being very pushy and calling every day, I would not have been offered continuing treatment in that first 7 months while I waited to see a consultant, even with a prior MS diagnosis and being on a first line approved treatment. That's a problem.
If two months is too long to wait to start DMT, how about four years? My first attack was November 2000. I had an MRI in December 2000 but didn't get the results until January 2001. I was told it was a relapsing-remitting condition. MS wasn't mentioned. I wasn't advised to have further tests, or to go back to my GP and ask for a referral to a specialist. Life went on as normal, with minor relapses, until I had a significant relapse in February 2004. I went to my GP who told me that the MRI had indicated 'probable MS'. He got me an appointment with a neurologist at the local hospital who confirmed the diagnosis, but didn't offer DMT. I had a major relapse that started in August 2004 and lasted about nine months. After a course of steroids failed to help, I was referred to a neurologist at the QE in Birmingham. I started taking Betaferon in November 2004. Four years from first relapse to starting DMT. And that's ignoring the 10 years from optic neuritis to first relapse. I'm currently taking Gilenya which I started in 2009, thanks to my neurologist putting me on the clinical trial.
The major relapse in 2004 left me with balance issues, speech problems when I get tired, and my left hip and thigh muscles are weaker than the right. My eyesight gets worse as the day goes on, so I don't drive at night. I have developed spasticity in both calves and in my right foot. I'd love to be able to sue the local hospital over the delay in getting me to see a specialist, but they'd claim best practice at the time, or that I should have seen my GP if I was concerned - except that I didn't know that I needed to be concerned! I know that I'm not badly off compared to many other pwMS, but I can't help wondering how I'd be if I had seen a neurologist sooner.
I find it ridiculous, but realise it’s a money issue, that MRIs for pwMS on NHS are only on the head. I had several relapses with spinal lesions. I was living in Europe at the time so had spinal MRIs. Even telling British neuros that I’m having issues similar to previous ones caused by plaques on my spine, they shrug and say ‘We don’t do spinal MRIs here’
I wasnt diagnosed for EIGHT years and only then because I went private! Despite having three nasty relapses…bladder, severe fatigue, swallowing and paralysis of right side (and numerous other symptoms) but was diagnosed with ME and depression. Once I was finally diagnosed with MS I started an interferon within six months and then finally onto Tysabri 6years later. I gave now been on Tysabri for over ten years with no obvious relapses.
I do occasionally think what may've happened if I had be diagnosed earlier tather than misdiagnosed with ME. I am still under the neurologist who diagnosed me but I see him on the NHS….he was my lifesaver.
I believe I may be able to beat all comments I was diagnosed in 2008 at age 47 after many years of what is named as hidden symptoms and numerous visits to my G.P. .Had a appointment with the Neurologist and after many tests was diagnosed with M.S. I was then informed there was no need to start treatment as very few were available ( which I now know to be untrue) and as I seemed ok he didn't see the need to start treatment?? Fast forward another another 9 years problems with mobility bladder and numerous other problems I was then offered Ocrevus I am now 62 and have two crutches but am only able to go to hospital appointments because of massive mobility and balance issues and as I have had a few bad falls because of this have lost any confidence am I bitter about my treatment yes extremely so as I am always thinking " if only"i am aware there are so many less fortunate and to them my heart goes out bless you all but I can only think would my dissability be as bad if I had the correct treatment? We will never know
Thank you for highlighting this, Prof G.
I had undiagnosed MS for 25 years. I originally had pediatric MS. I was severely disabled the entire time. The NHS put me on anti-depressants and told me I had Chronic Fatigue Syndrome.
The NHS never diagnosed me and never would have. I had no access to Healthcare on the NHS. I begged for a referral to a neurologist and an MRI scan, and was told no. I only have a diagnosis because far too late I gave up on the NHS, diagnosed myself via Google, went private and put it on credit card.
I'm left with significant cerebral atrophy and PTSD, trying to find a way to live with what the NHS has done to me. I was too traumatized to make complaints (time limit a year) or sue (3 years). I wish the NHS cared what it had done and would change. But it doesn't and won't.
Yes, after I paid to finally see a neurologist, it was a year till I started a DMT (Plegridy, with no other options). But the much bigger problem is that I was denied access to a diagnosis for a quarter of a century, and it can't just be me.
Hi Prof G
So, time is of the essence is it? I wish it was.
I'm PP- not RR-MS so my apologies for crashing this particular party, but my MS Consultant still adopted a wait-and-see ("watchful waiting?") approach to treatment in spite of a misdiagnosis stretching back at least 6 years. Following first consult I already scored at EDSS6.0 (retrospectively self-scored at EDSS1 6 years ago, so quite aggressive) and 15 months later, the only medication I'm receiving is Baclofen!
I'm one of your "smouldering" brigade (NEIDA) and still have no treatment plan other than a referral to Urology and a couple of MRI's. Not good enough!
I think the issue, for me at least, was understanding I had MS
Eg my first symptoms where MS hug and parasthesia in my hands (which I still have)
Eliminating typical blood work possibilities, carpal tunnel and getting in to see a neurologist took time. It was for me 2 months from symptoms onset to neurologist confirmation of MS
Then another 7 weeks to start Tysabri due to waiting for JC results as they go from Australia to Denmark at unilabs.
All in all if there was an instant test (blood work) available you could start treatment within 2 weeks or sooner.
I don't think I took too long to start but recognise I ignored my neck Lhermittes sign symptoms for about 12 months (typical male thought it was nothing)
Overall time to treatment was 5 months.
And I don't fault the Drs here as it was a process of elimination and covid unfortunately
Hi Prof G, Thank you for the opportunity to look on your MS-Selfie site.
As a Newly diagnosed patient with MS on 4/11/22 I was informed by my Neurologist I had MS , I did not need a lumbar puncture, due to damage already present but another MRI with contrast. I was advised I would be referred to the MS clinic for further management.
I had MRI scan before Christmas and last week had a letter advising me of the results. These were not clear I’m a healthcare professional and I did not understand what was being said, I asked my Gp who advised you will have to ask the neurologist.
I still don’t have an appointment date for the clinic so can’t seen it being in the near future.
Months into diagnosis I have no idea of the type of Ms I have or what treatment options may be available.
I have been symptomatic for 4years initially with balance problems and then fatigue, unfortunately was diagnosed with chronic fatigue and at the time I was active for EBV.
After 12 months fatigue had gone but more neurological symptoms appeared after speaking to Gp who said It was low Vitamin D even though I took vitamin D supplements every day I waited 3 months nothing had changed and I started falling over. Finally agreed to send me to a neurologist 5 month wait . With a lovely neurologist within 8 weeks I had my diagnosis.
I feel it is a disjointed service. The NHS is under massive pressures I work for them so understand but the selfish part of me want to get onto a DMT if possible to reduce some of the episodes I have. Every 8-12 weeks I have new symptoms appear done stay some go.
I want to be a patient that takes control but can’t.
Starting treatment within 2weeks of diagnosis would be life changing for MS patients.
You are doing amazing work, I have subscribed
A massive Thank you I definitely have a better understanding of MS now
Sarah
Thank you for subscribing it is much appreciated.
It's interesting to see the US and UK struggling with the same issues of delayed diagnosis and treatment. The UK delays seem more related to the NHS processes. Whereas here in the US, many of the delays in MS diagnosis and treatment can be attributed to disparities in care, lack of access to expert care, and a significant deficiency of knowledge about MS in the medical community. I love the aspirations of the AttackMS trial and the International Quality Standards to push the bar to improve these timelines and outcomes for MS patients. I appreciate Prof G's hard work and accomplishments. I am a neuro Nurse Practitioner who specializes in MS care who also has MS. I was diagnosed 20years ago. I definitely consider myself one of the lucky ones who benefitted from early diagnosis and expert care. Now it's time for me to advocate for all those who are not so lucky. Keep up the good work Prof. G.
Sadly the NHS doesn’t have much knowledge of MS (Dr G exception-but he wasn’t trained via NHS)
Can you please get the US to adopt these standards too? These would be amazing
How long til results of the attack ms trial? Love the hypothesis and the study design could be huge. Ms diagnosis and treatment needs a kick in the pants. Maybe borrow urgency from the oncology playbook
But what about those MSers who do not have 2 incidents of prolonged activity and symptoms? I was diagnosed in March 2019 and my MRIs have always been grossly stable (the radiologists terminology not mine). I have had disruptive trips and walking fatigue since my early 30's, but I manage fairly well. My management of my MS by my team is most definitely 'watch and wait'. I do not fit the criteria, or qualify for treatment, under the NICE guidelines. Everyone tells me I should be on a treatment, but I mange well enough with my diet, exercise and mediation. My MS Neuro and MS Nurse yesterday told me they would see me in 2023. Fine by me. Life is treating me well. What's more for a girl to do?!
Yes, you are right. If you have inactive MS then you are not eligible for treatment under current treatment guidelines. Keep doing what you do.
I continue to believe we should put people on DMTs *before* diagnosis.
The McDonald diagnosis criteria are very conservative and the MS doctors even more so. So often MS people say they had MS symptoms years/decades before diagnosis.
And yet research is showing that an early start to DMTs can make a huge difference to the long-term curve of the disease decades later.
We could put people on DMTs as as soon as first possible MS signs show (fatigue I suspect, in many cases). They could then come off DMTs later, if MS was found not to be occurring.
We might start with people showing symptoms who also have other MS risk factors (e.g. have another automimmune disease, and/or genetic inheritance).
Yes meds are expensive - but the long-term health economics payback would be hugely positive I think - let alone the direct and collateral savings of long-term human suffering.
I was initially diagnosed idiopathic neuropathy. 9 months later, after my body went into free fall, was finally diagnosed MS and immediately prescribed Tysaberi.
In hindsight, my first neurologist missed all the classic symptoms. And yes, I believe those 9 missed months cost me a lot.
Thank you Dr. G!
How about a post on Thymosin Alpha One??!!
Why is PPMS never the subject matter of this blog? I have PPMS and it appears as the also ran"
I don't think PPMS is a different disease. MS is one disease you either have MS or you don't have MS. Referring to PPMS as if it is was a different disease exacerbates the problems we have in getting MS treated.
'"MS is one disease"
I think this is a very valid point that needs to be more widely known. Offering DMTs that are only for people with RRMS skews the figures and those diagnosed with SPMS are consigned to the dustbin. Acceptance that MS is one disease will stop exclusion and inequities. Is this as important as flipping the pyramid?
I try not to focus on the 'consigned to the dustbin' part but it is true.
This is exactly what my neurologist says. He hates the labels of MS.
He says this DMT will work or it won't and we can try them. If you limit it to what's "approved" for the MS sub type you don't help the patient
A good point!
I was diagnosed in Aberdeen in 2016 and was essentially given my diagnosis in a letter (which was awful) then in a consultation with the neuro said there was nothing they could do for me (that relapse was a numb leg but I had optic neuritis in 2012). I asked about medications and he said they weren't for me. I asked about regular scans and he said just come back if you have another problem and he sent me on my way.
I trusted the authority of the neuro and went away not very happy but I figured he knew best. 3 years later I had moved to edinburgh, had a massive relapse (numb from neck down, weakness in both hands). It greatly angers me that I may be in a better position had I been put on medication earlier. As soon as I saw the neuro in Edinburgh they got me onto a DMT and were well aware of the poor care that was being given in Aberdeen. Is there a way we can change this as a patient group?
Interesting stuff. Might it be possible to write a post about when, why and how to switch neurologists?
The picture will no doubt be very different in different countries and - in the UK at least - postcodes. If you have the money for good insurance in the US I think it's a bit easier - though the situation is awful for those on low incomes. I presume there's similarly unjust division of care elsewhere. In the UK, I think you're at the mercy of your postcode.
I am I presume a privileged NHS patient in that I live in London, where – I'm guessing again – patients can request a transfer, but I have no idea what the systematic/diplomatic approach should be.
I'm 53 and shading into the age band where prescriptions become more conservative.
I have little to complain about where I am treated, really, but their approach is more conservative than I would wish for – and it took 4/5 years of asking to get switched from copaxone to alemtuzumab. I don't doubt there are good arguments for a conservative approach. But I would like to be treated more ambitiously (sadly had to be excluded from the SIZOMUS trial.)
It seems possible that I might have kept hold of stereo eyesight if my hospital had been a little less cautious, and I don't want to waste another 4/5 years of time/brain if effective treatments become available in the nearish future.
Sorry to bang on about my own circumstances, which are relatively lucky, and I do believe in the NHS principle that I should not receive any better care than someone down the road – despite the ridiculous insistence on treating NHS patients, who are relentlessly invited to 'recommend' their hospital over others, like shoppers. But I suspect this would be a question of general interest - even if your expert view is that you should stick with what you have.
Thanks for reading.