A recent paper from two U-M hepatologists highlights the liver dangers associated with consuming some herbal and dietary supplements designed to build muscle or lose weight.
7:00 AM
Author |

Athletes often use over-the-counter products to help lose weight or improve their energy and performance levels.
However, the vast majority of herbal and dietary supplements (HDS) never undergo formal efficacy or safety tests because their manufacturing, production and content are not closely regulated by the Food and Drug Administration, says Robert Fontana, M.D., University of Michigan's medical director of liver transplantation, and Ammar Hassan, M.D., a U-M hepatology fellowship graduate, who have explored several over-the-counter HDS products linked to liver injury.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
As the number of HDS products available in the United States continues to grow, more than 80,000 commercial products are available to consumers, with nearly 50 percent of adults reporting regular use of at least one kind of supplement. Many adverse effects are linked to consuming HDS products, including hepatotoxicity, or chemically induced liver damage, according to the Drug-Induced Liver Injury Network.
Fontana and Hassan explored several popular over-the-counter HDS products linked to liver injury in a recent article in Seminars in Liver Disease. Here is a rundown:
Bodybuilding supplement hepatotoxicity
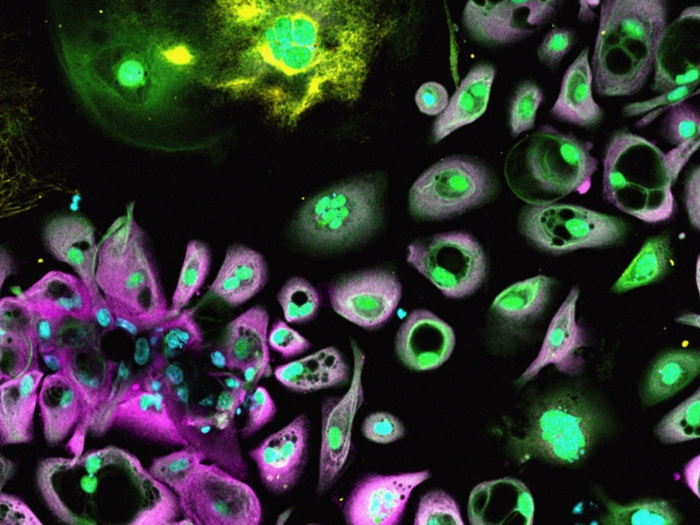
The majority of bodybuilding HDS products that lead to liver injury appear to contain androgenic anabolic steroids (AAS) or are contaminated with these and other chemicals.
AAS are synthetic derivatives of testosterone. Some medical conditions require the use of AAS products, including primary male hypogonadism and hereditary angioneurotic edema, but athletes use many of these steroids without medical supervision for their performance-enhancing and muscle-building properties.
SEE ALSO: Troubling Trends in Drug-Induced Liver Damage
"The use of these products is very common among amateur and professional athletes, including many active-duty military personnel," Fontana says. "Data suggests that 69 percent of these individuals use at least one HDS product, while 22 percent report using more than three a day."
These products are often purchased at health food stores or online in bulk. Over the past two decades, a significant increase in the incidence of liver injury related to the illicit use of AAS has been reported.
"Bodybuilding supplements that contain AAS can lead to liver damage, including severe cholestatic hepatitis, which can take months to resolve," Fontana says. "Additionally, various multi-ingredient nutritional supplements taken to enhance energy, increase performance and facilitate weight loss can lead to potentially severe, or even fatal, liver damage."
Non-bodybuilding supplement hepatotoxicity
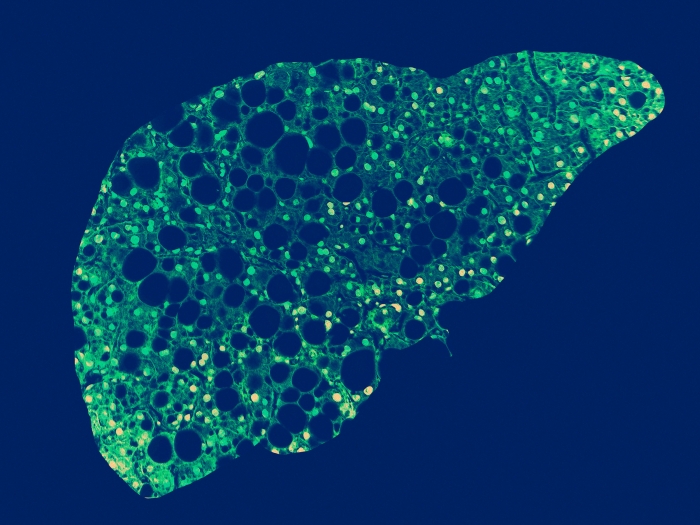
Some of the most frequently used non-bodybuilding supplements associated with hepatotoxicity include green tea extract and multi-ingredient nutritional supplements that contain both botanicals and other compounds. These products include familiar names like Hydroxycut, Oxy ELITE Pro and LipoKinetix.
Green tea extract, or GTE, is derived from unfermented leaves of the Chinese tea tree, Camellia sinensis. One of the active ingredients in GTE is epigallocatechin gallate, which is a catechin, or a compound that is abundant in teas, cocoa products and certain berries. It boasts purported weight-loss properties by stopping fat-causing lipogenic enzymes.
While the public tends to view HDS products as safer than most conventional medications because they are derived from plants and other "natural sources," this is not always the case, Fontana says.
"Various animal studies have shown the hepatotoxic (and possibly deadly) potential of GTE," he says. "Extreme levels of GTE will lead to elevated aminotransferase (enzymes) in mice that significantly reduce their survival rates."
Further, the Drug-Induced Liver Injury Network reported a study in which six patients who took GTE-containing Slimquick weight-loss products suffered hepatocellular injury, while four of the six were also severely jaundiced. Additionally, three patients from this group were hospitalized, and one had to have a liver transplant.
Hydroxycut hepatotoxicity
The first reported incidents of hepatotoxicity attributed to ephedra-containing Hydroxycut involved 12 patients in the U.S. who developed severe hepatitis after consuming supplements. Of the patients, 75 percent were female, with a mean age of 38.
It took an average of just eight weeks for an individual to develop hepatocellular injury after taking Hydroxycut.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Eight of these patients recovered from their liver damage, while three underwent liver transplantation, Fontana says. One patient died before transplantation.
At least 17 additional cases of Hydroxycut-associated liver injury have been reported with similar phenotypes of liver injury and outcomes. And in 2004, the FDA banned the sale of supplements containing ephedra.
In May 2009, the FDA published a warning about Hydroxycut-related hepatotoxicity, resulting in withdrawal of 14 Hydroxycut products from the market.
"Without regulations like standardized chemical analyses and product manufacturing guidelines, it is nearly impossible to determine the exact chemical makeups for these types of supplements," Fontana says. "And that just adds another element of danger to consuming them."
Fontana has received research grants from AbbVie, Gilead Sciences and Bristol-Myers Squibb. He also provides consulting services for Alnylam Pharmaceuticals.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!