Abstract
Seasonal influenza viruses constantly change through antigenic drift and the emergence of pandemic influenza viruses through antigenic shift is unpredictable. Conventional influenza virus vaccines induce strain-specific neutralizing antibodies against the variable immunodominant globular head domain of the viral hemagglutinin protein. This necessitates frequent re-formulation of vaccines and handicaps pandemic preparedness. In this completed, observer-blind, randomized, placebo-controlled phase I trial (NCT03300050), safety and immunogenicity of chimeric hemagglutinin-based vaccines were tested in healthy, 18–39-year-old US adults. The study aimed to test the safety and ability of the vaccines to elicit broadly cross-reactive antibodies against the hemagglutinin stalk domain. Participants were enrolled into five groups to receive vaccinations with live-attenuated followed by AS03-adjuvanted inactivated vaccine (n = 20), live-attenuated followed by inactivated vaccine (n = 15), twice AS03-adjuvanted inactivated vaccine (n = 16) or placebo (n = 5, intranasal followed by intramuscular; n = 10, twice intramuscular) 3 months apart. Vaccination was found to be safe and induced a broad, strong, durable and functional immune response targeting the conserved, immunosubdominant stalk of the hemagglutinin. The results suggest that chimeric hemagglutinins have the potential to be developed as universal vaccines that protect broadly against influenza viruses.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The protocol, statistical analysis plan and results will be available at https://clinicaltrials.gov/ct2/show/NCT03300050. Underlying data are available upon request (excluding identifiable information).
References
Palese, P. Influenza: old and new threats. Nat. Med. 10, S82–S87 (2004).
Chan, M. C. W. et al. Frequent genetic mismatch between vaccine strains and circulating seasonal influenza viruses, Hong Kong, China, 1996–2012. Emerg. Infect. Dis. 24, 1825–1834 (2018).
Flannery, B. et al. Spread of antigenically drifted influenza A(H3N2) viruses and vaccine effectiveness in the United States during the 2018–2019 season. J. Infect. Dis. 221, 8–15 (2020).
Skowronski, D. M. et al. Paradoxical clade- and age-specific vaccine effectiveness during the 2018/19 influenza A(H3N2) epidemic in Canada: potential imprint-regulated effect of vaccine (I-REV). Euro Surveill. 24, 1900585 (2019).
Owusu, D. et al. Early season pediatric influenza B/Victoria virus infections associated with a recently emerged virus subclade—Louisiana, 2019. MMWR Morb. Mortal. Wkly Rep. 69, 40–43 (2020).
Virk, R. K. et al. Divergent evolutionary trajectories of influenza B viruses underlie their contemporaneous epidemic activity. Proc. Natl Acad. Sci. USA 117, 619–628 (2020).
Krammer, F. & Palese, P. Advances in the development of influenza virus vaccines. Nat. Rev. Drug Discov. 14, 167–182 (2015).
Krammer, F. The human antibody response to influenza A virus infection and vaccination. Nat. Rev. Immunol. 19, 383–397 (2019).
Hobson, D., Curry, R. L., Beare, A. S. & Ward-Gardner, A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. (Lond.) 70, 767–777 (1972).
Heaton, N. S., Sachs, D., Chen, C. J., Hai, R. & Palese, P. Genome-wide mutagenesis of influenza virus reveals unique plasticity of the hemagglutinin and NS1 proteins. Proc. Natl Acad. Sci. USA 110, 20248–20253 (2013).
Doud, M. B. & Bloom, J. D. Accurate measurement of the effects of all amino-acid mutations on influenza hemagglutinin. Viruses 8, 155 (2016).
Kirkpatrick, E., Qiu, X., Wilson, P. C., Bahl, J. & Krammer, F. The influenza virus hemagglutinin head evolves faster than the stalk domain. Sci. Rep. 8, 10432 (2018).
Okuno, Y., Isegawa, Y., Sasao, F. & Ueda, S. A common neutralizing epitope conserved between the hemagglutinins of influenza A virus H1 and H2 strains. J. Virol. 67, 2552–2558 (1993).
Wu, N. C. & Wilson, I. A. Structural insights into the design of novel anti-influenza therapies. Nat. Struct. Mol. Biol. 25, 115–121 (2018).
Corti, D. et al. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science 333, 850–856 (2011).
Dreyfus, C. et al. Highly conserved protective epitopes on influenza B viruses. Science 337, 1343–1348 (2012).
Ng, S. et al. Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nat. Med. 25, 962–967 (2019).
Dilillo, D. J., Tan, G. S., Palese, P. & Ravetch, J. V. Broadly neutralizing hemagglutinin stalk-specific antibodies require FcγR interactions for protection against influenza virus in vivo. Nat. Med. 20, 143–151 (2014).
Brandenburg, B. et al. Mechanisms of hemagglutinin targeted influenza virus neutralization. PLoS ONE 8, e80034 (2013).
Rajendran, M. et al. Analysis of anti-influenza virus neuraminidase antibodies in children, adults, and the elderly by ELISA and enzyme inhibition: evidence for original antigenic Sin. mBio 8, e02281–16 (2017).
Hai, R. et al. Influenza viruses expressing chimeric hemagglutinins: globular head and stalk domains derived from different subtypes. J. Virol. 86, 5774–5781 (2012).
Margine, I. et al. Hemagglutinin stalk-based universal vaccine constructs protect against group 2 influenza A viruses. J. Virol. 87, 10435–10446 (2013).
Krammer, F., Pica, N., Hai, R., Margine, I. & Palese, P. Chimeric hemagglutinin influenza virus vaccine constructs elicit broadly protective stalk-specific antibodies. J. Virol. 87, 6542–6550 (2013).
Nachbagauer, R. et al. A universal influenza virus vaccine candidate confers protection against pandemic H1N1 infection in preclinical ferret studies. NPJ Vaccines 2, 26 (2017).
Choi, A. et al. Chimeric hemagglutinin-based influenza virus vaccines induce protective stalk-specific humoral immunity and cellular responses in mice. Immunohorizons 3, 133–148 (2019).
Nachbagauer, R. et al. A chimeric haemagglutinin-based influenza split virion vaccine adjuvanted with AS03 induces protective stalk-reactive antibodies in mice. NPJ Vaccines 1, 16015 (2016).
Nachbagauer, R. et al. Age dependence and isotype specificity of influenza virus hemagglutinin stalk-reactive antibodies in humans. mBio 7, e01996–15 (2016).
Sui, J. et al. Wide prevalence of heterosubtypic broadly neutralizing human anti-influenza A antibodies. Clin. Infect. Dis. 52, 1003–1009 (2011).
Bernstein, D. I. et al. Immunogenicity of chimeric haemagglutinin-based, universal influenza virus vaccine candidates: interim results of a randomised, placebo-controlled, phase 1 clinical trial. Lancet Infect. Dis. 20, 80–91 (2020).
Talaat, K. R. et al. A live attenuated influenza A(H5N1) vaccine induces long-term immunity in the absence of a primary antibody response. J. Infect. Dis. 209, 1860–1869 (2014).
Rudenko, L. et al. Assessment of immune responses to H5N1 inactivated influenza vaccine among individuals previously primed with H5N2 live attenuated influenza vaccine. Hum. Vaccin. Immunother. 11, 2839–2848 (2015).
Barría, M. I. et al. Localized mucosal response to intranasal live attenuated influenza vaccine in adults. J. Infect. Dis. 207, 115–124 (2013).
Lee, J. et al. Molecular-level analysis of the serum antibody repertoire in young adults before and after seasonal influenza vaccination. Nat. Med. 22, 1456–1464 (2016).
Ekiert, D. C. et al. Cross-neutralization of influenza A viruses mediated by a single antibody loop. Nature 489, 526–532 (2012).
Khurana, S. et al. MF59 adjuvant enhances diversity and affinity of antibody-mediated immune response to pandemic influenza vaccines. Sci. Transl. Med. 3, 85ra48 (2011).
Ekiert, D. C. et al. Antibody recognition of a highly conserved influenza virus epitope. Science 324, 246–251 (2009).
Sui, J. et al. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat. Struct. Mol. Biol. 16, 265–273 (2009).
Nachbagauer, R. et al. Induction of broadly reactive anti-hemagglutinin stalk antibodies by an H5N1 vaccine in humans. J. Virol. 88, 13260–13268 (2014).
Ellebedy, A. H. et al. Induction of broadly cross-reactive antibody responses to the influenza HA stem region following H5N1 vaccination in humans. Proc. Natl Acad. Sci. USA 111, 13133–13138 (2014).
Jacobsen, H. et al. Influenza virus hemagglutinin stalk-specific antibodies in human serum are a surrogate marker for in vivo protection in a serum transfer mouse challenge model. mBio 8, e01463–17 (2017).
Bangaru, S. et al. A site of vulnerability on the influenza virus hemagglutinin head domain trimer interface. Cell 177, 1136–1152.e1118 (2019).
Watanabe, A. et al. Antibodies to a conserved influenza head interface epitope protect by an IgG subtype-dependent mechanism. Cell 177, 1124–1135.e1116 (2019).
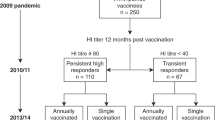
Nachbagauer, R. et al. Pandemic influenza virus vaccines boost hemagglutinin stalk-specific antibody responses in primed adult and pediatric cohorts. NPJ Vaccines 4, 51 (2019).
He, W. et al. Alveolar macrophages are critical for broadly-reactive antibody-mediated protection against influenza A virus in mice. Nat. Commun. 8, 846 (2017).
Chromikova, V. et al. Activity of human serum antibodies in an influenza virus hemagglutinin stalk-based ADCC reporter assay correlates with activity in a CD107a degranulation assay. Vaccine 38, 1953–1961 (2020).
Cohet, C. et al. Safety of AS03-adjuvanted influenza vaccines: a review of the evidence. Vaccine 37, 3006–3021 (2019).
Krammer, F. et al. H3 stalk-based chimeric hemagglutinin influenza virus constructs protect mice from H7N9 challenge. J. Virol. 88, 2340–2343 (2014).
Sun, W. et al. Development of influenza B universal vaccine candidates using the ‘mosaic’ hemagglutinin approach. J. Virol. 93, e00333–19 (2019).
Pitisuttithum, P. et al. Safety and immunogenicity of a live attenuated influenza H5 candidate vaccine strain A/17/turkey/Turkey/05/133 H5N2 and its priming effects for potential pre-pandemic use: a randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 17, 833–842 (2017).
Isakova-Sivak, I. et al. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology 412, 297–305 (2011).
Isakova-Sivak, I. et al. Broadly protective anti-hemagglutinin stalk antibodies induced by live attenuated influenza vaccine expressing chimeric hemagglutinin. Virology 518, 313–323 (2018).
Rajendran, M. et al. An immuno-assay to quantify influenza virus hemagglutinin with correctly folded stalk domains in vaccine preparations. PLoS ONE 13, e0194830 (2018).
Martínez-Sobrido, L. & García-Sastre, A. Generation of recombinant influenza virus from plasmid DNA. J. Vis. Exp. 3, 2057 (2010).
Hong, M. et al. Antibody recognition of the pandemic H1N1 influenza virus hemagglutinin receptor binding site. J. Virol. 87, 12471–12480 (2013).
Margine, I., Palese, P. & Krammer, F. Expression of functional recombinant hemagglutinin and neuraminidase proteins from the novel H7N9 influenza virus using the baculovirus expression system. J. Vis. Exp. 6, e51112 (2013).
Impagliazzo, A. et al. A stable trimeric influenza hemagglutinin stem as a broadly protective immunogen. Science 349, 1301–1306 (2015).
Bliss, C. M. et al. Targeting antigen to the surface of EVs improves the in vivo immunogenicity of human and non-human adenoviral vaccines in mice. Mol. Ther. Methods Clin. Dev. 16, 108–125 (2020).
Stadlbauer, D. et al. Broadly protective human antibodies that target the active site of influenza virus neuraminidase. Science 366, 499–504 (2019).
Wang, G. et al. Characterization of swine-origin H1N1 canine influenza viruses. Emerg. Microbes Infect. 8, 1017–1026 (2019).
Chromikova, V., Zaragoza, M. A. & Krammer, F. Generation of a serum free CHO DG44 cell line stably producing a broadly protective anti-influenza virus monoclonal antibody. PLoS ONE 12, e0183315 (2017).
McMahon, M. et al. Vaccination with viral vectors expressing chimeric hemagglutinin, NP and M1 antigens protects ferrets against influenza virus challenge. Front. Immunol. 10, 2005 (2019).
Lu, Y. et al. Immune response to influenza vaccine in children with inflammatory bowel disease. Am. J. Gastroenterol. 104, 444–453 (2009).
Treanor, J. et al. Safety and immunogenicity of a baculovirus-expressed hemagglutinin influenza vaccine: a randomized controlled trial. JAMA 297, 1577–1582 (2007).
Acknowledgements
We thank the research team at the Department of Microbiology at the Icahn School of Medicine at Mount Sinai for supporting the development of this vaccine concept since 2011. We also thank the teams at PATH (with special acknowledgement to J.C. Victor, R. Wahid and K. Mahmood), Cincinnati Children’s Hospital Medical Center, Duke University, the University of Chicago, GSK, NEOMED-LABS and the EMMES Corporation for their work on this project. We are grateful for help from V. Simon at Mount Sinai with IRB protocol development, D. Wentworth and L. M. Chen at the US CDC with the initial LAIV seed virus rescue and for help from D. Suarez from the US Department of Agriculture for pathogenicity testing of the vaccine virus strains. We thank G. Georgiou for providing monoclonal antibody D1 H1-3/H3-3 used in competition ELISAs. This study was funded in part by the Bill and Melinda Gates Foundation (grant OPP1084518). Basic research leading to this trial was supported by the National Institute of Allergy and Infectious Diseases (NIAID) (grants P01 AI097092, HHSN26620070010C, HHSN272201400008C, U19 AI109946, R01 AI128821). NIAID continues to support analysis of samples from this trial through a Collaborative Influenza Vaccine Innovation Centers contract (75N93019C00051). GSK made adjuvants and vaccine preparations available and contributed through providing expertise as well (funding for this study was provided by GlaxoSmithKline Biologicals SA). The findings and conclusions contained within are those of the authors and do not necessarily reflect positions or policies of the Gates Foundation. GlaxoSmithKline Biologicals SA was provided the opportunity to review a preliminary version of this manuscript for factual accuracy, but the authors are solely responsible for final content and interpretation.
Author information
Authors and Affiliations
Contributions
J.F., A.N., D.I.B., J.G., E.B.W., F.B.-S., C. Claeys, C.G., C.M., M.M.N., A.S., M.V.d.W. and B.L.I. are responsible for conducting, managing and coordinating the clinical trial. Laboratory experiments were performed by R.N., D.S., T.A., M.A.B., D.B., C.B., C. Capuano, J.M.C., V.C., L.C., A.W.F., A.J., K.J., M.M.M., M.M.N., S.S. and W.S. Resources and methods were provided by L.C., T.A., W.S., A.W.F., V.C., S.S., P.C.W. and F.K. All authors are responsible for writing, reviewing and editing the manuscript. Data analysis was performed by R.N., J.F., A.N., F.B.-S., D.S., J.M.C., V.C., C.G., C.M., A.S., B.L.I., A.G.-S., P.P. and F.K. Quality assurance on assays was performed at ISMMS by C.M.
Corresponding author
Ethics declarations
Competing interests
The Icahn School of Medicine at Mount Sinai (ISMMS) has issued patents and filed patent applications covering the use of chimeric hemagglutinin antigens as vaccines. R.N., A.G.-S., P.P. and F.K. are named as inventors on these patents and applications. The ISMMS and the inventors have received payments as consideration for these rights. The laboratories of A.G.-S., P.P. and F.K. were also engaged in a research program that was funded by GlaxoSmithKline Biologicals SA. M.V.d.W. declares that she is employed by the GSK group of companies and declares no nonfinancial conflicts of interest. C. Claeys was an employee of the GSK group of companies at the time the study was performed. B.L.I. was an employee of the GSK group of companies until 2017 and held shares from this group of companies at the time the study was performed. He is also named as inventor on a patent family regarding influenza virus vaccine constructs filed by the ISMMS and the GSK group of companies. E.B.W. is a coinvestigator for a clinical trial supported by Pfizer. All other authors declare no competing interests.
Additional information
Peer review information Alison Farrell is the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Microneutralization titers.
Microneutralization titers against cH6/1N5 virus (a), pandemic H1N1 virus (c), avian-swine H1N1 virus (e) and H5N8 virus (g). Faint lines indicate reactivity of different individuals; bold lines indicate geometric mean titers of the respective groups. Biologically independent samples; group 1: n = 19, group 2: n = 14, group 4: n = 15 groups 3 + 5: n = 13(3 + 10); examined in one independent experiment. Geometric mean fold induction of antibody titers based on data in a, c, e and g is shown in b, d, f and h.
Extended Data Fig. 2 Hemagglutination inhibition (HI) titers.
Hemagglutination inhibition titers against cH6/1N5 virus (a), pandemic H1N1 virus (c), avian-swine H1N1 virus (e) and H5N8 virus (g) as well as cH8/1N1 (I) and cH5/1N1 (k) vaccine strains. Faint lines indicate reactivity of different individuals; bold lines indicate geometric mean titers of the respective groups. Biologically independent samples; group 1: n = 19, group 2: n = 14, group 4: n = 15 groups 3 + 5: n = 13(3 + 10); examined in one independent experiment. Geometric mean fold induction of antibody titers based on data in a, c, e, g, i and k is shown in b, d, f, h, j and l.
Supplementary information
Supplementary Information
Supplementary Figs. 1–10 and Supplementary Tables 1–3.
Rights and permissions
About this article
Cite this article
Nachbagauer, R., Feser, J., Naficy, A. et al. A chimeric hemagglutinin-based universal influenza virus vaccine approach induces broad and long-lasting immunity in a randomized, placebo-controlled phase I trial. Nat Med 27, 106–114 (2021). https://doi.org/10.1038/s41591-020-1118-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-1118-7
This article is cited by
-
Structurally convergent antibodies derived from different vaccine strategies target the influenza virus HA anchor epitope with a subset of VH3 and VK3 genes
Nature Communications (2025)
-
Pathogens and planetary change
Nature Reviews Biodiversity (2025)
-
Chimeric hemagglutinin and M2 mRNA vaccine for broad influenza subtype protection
npj Vaccines (2025)
-
Use standard and enhanced vaccines to prevent influenza, while new classes remain in development
Drugs & Therapy Perspectives (2025)
-
Next-generation vaccines for influenza B virus: advancements and challenges
Archives of Virology (2025)