If and when New Zealand exits alert level four and its restrictions, contact tracing becomes the most important tool we have to prevent having to lockdown all over again. So what does it involve, and are we doing enough of it?
Just quickly – what is contact tracing?
Contact tracing is what happens to determine which people a probable or confirmed case has been in contact with, and how closely. There are two main focuses for contact tracing: close contacts and casual contacts.
The first group is much more important to trace, because if someone has Covid-19, their close contacts have a higher likelihood of also having it. Close contacts range along a spectrum from those who have had direct contact with the bodily fluid of an infected person, to having sat within two metres of them for more than 15 minutes.
A casual contact is described as “any person with exposure to the case who does not meet the criteria for a close contact”. That could mean sitting on the same plane, but four rows of seats back, for example. Casual contacts are much less likely to pick up Covid-19 from an infected person, but it is still possible. That’s a big part of the reason events like Polyfest and the March 15 commemorations in Christchurch were cancelled last month – there would simply have been far too many casual and close contacts to trace, made harder by the fact they’re unticketed events.
Those who have been in close contact with a confirmed or suspected case of Covid-19 need to go into self-isolation immediately, and monitor themselves for symptoms for 14 days.
So how does the contact tracing actually work?
At the moment, it involves people with confirmed or probable cases saying where they’ve been, for how long and with whom over a period of time, and then health workers try and get in touch with all of those people. A couple of different groups are currently working on this. The first group is staff at Public Health Units attached to DHBs, and the second is the new workforce attached to the National Close Contact Service, which is part of the Ministry of Health.
The standard process for this has been a two-stage process, by which a person is first interviewed by a case manager to get their details, and then contact tracers follow up with those people who are named. As you can probably imagine, it’s not flawless – someone might forget a contact, or forget someone’s name in the original interview, meaning that a potential close contact can’t be followed up.
And how is it all going so far?
That depends who you ask. “As of Saturday, 4,909 close contacts had been traced by the NCCS since it was stood up on March 24, with 702 contacts traced in a single day on Thursday,” said NZ’s director of public health Dr Caroline McElnay in a Sunday media release. “Originally it was making 760 calls a day – now that’s more than 2,000.”
Those numbers might sound like a lot, and they’re certainly moving in the right direction. But Otago University public health expert Dr Ayesha Verrall says while the increase in capacity is really good, there are still unanswered questions.
Such as?
“The speed is really important, and whether we can be fast enough with the tools that we have,” Verrall told The Spinoff. If a contact isn’t traced for several days after being in contact with an infected person, that increases the likelihood that they in turn will unwittingly pass Covid-19 on.
The other issue Verrall highlighted was the scale, and whether it could be enlarged quickly. “I think they need to be able to trace about 1,000 cases a day. So they’re doing 700 contacts at the moment, but every case could have multiple contacts. At the moment, we will have very few contacts because we’re in small bubbles, but in the future that could increase, especially if we’re at level three.”
Why does this matter so much to the wider effort to fight Covid-19?
Theoretically, if we stayed in lockdown forever we’d barely need to scale up the contact tracing system. But that isn’t going to happen – and our ability to leave lockdowns (and stay out of them) will be determined how comprehensively we can do contact tracing. “It’s our fire extinguisher,” said Verrall, “and we want a giant fire extinguisher before we go into lockdown and hide from the fire.”
“Unless you know how many cases you can trace, you don’t know what your epidemiological trigger is for going into lockdown,” said Verrall. She offered some maths which put it into context.
“Let’s say we can trace 100 cases and their contacts a day – 700 contacts probably relates to about 100 cases, at about seven per case. So if we can trace 100 cases nationwide, that means the next time we have 100 new cases in a day we have to go into lockdown. We’re actually nearly at that already, because we’re getting 80 cases a day, so our current contact tracing capacity isn’t much better than our control of the outbreak. So it looks like we can’t leave lockdown any time soon.”
Bugger. What can be done to improve this all?
There are a few mechanisms which will increase the capacity, over and above the Ministry of Health and district health boards getting more staff tooled up and ready to go. One category is quite basic – we all just become a lot better at recording where we’ve been, and with who. For those who get a bit of a thrill from signing the visitor book at a Cosmopolitan Club in an unfamiliar town, expect that sort of system to be in place at every venue as we come out of lockdown, and the signing to be compulsory. If you went to a pub in the few days we were at alert level three, you should have been asked to sign in.
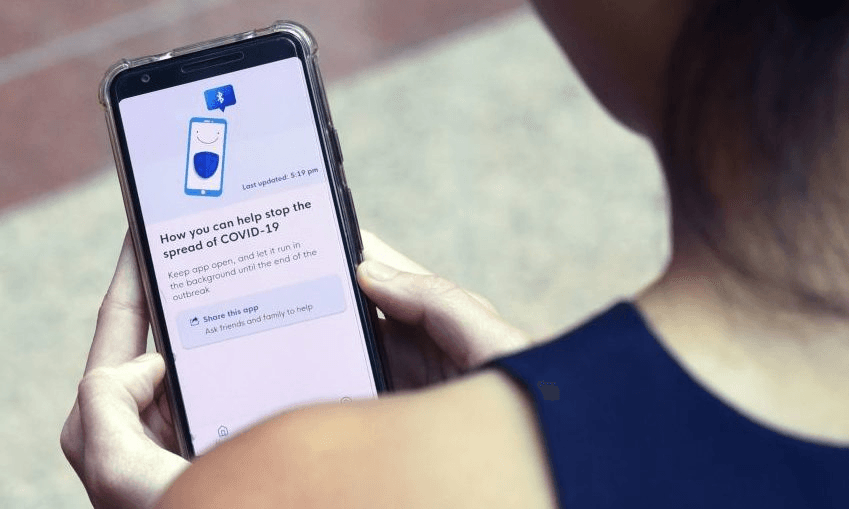
The other thing that could help a lot is an app, or some other digital service that automates a lot of this process. The government is currently working on just such an app, with mobile phone tracking capability. Given human memory is often flawed (saying you stopped to chat with “the guy in the mall in a stripy jumper” doesn’t quite cut it) this would dramatically increase the capacity of the contact tracing system – provided people signed up for it in large enough numbers. It would also allow automation – rather than someone having to call you when they get through their existing backlog, it could immediately send a message to all those who were on the same bus as a confirmed case, for example. A free app in Singapore – called Trace Together, is considered to be a world-leading piece of software, and has contributed to that country’s case numbers staying relatively low.
Isn’t cellphone tracking for this a bit creepy?
Such a system would raise serious privacy concerns. Auckland University’s Dr Andrew Chen has looked into this issue, arguing that while governments already have the legal ability to do this, there are ethical considerations with mass surveillance that need to be taken into account as well.
“Using cellphone data to track people for the purposes of contact tracing may be acceptable to some, but for others it will make them feel uncomfortable and undermine their confidence in government,” he said. “At a time when morale and trust in government are critical for stability and encouraging compliance, the risk of alienating people is a real concern.”
The Ministry of Health says it is taking these sorts of concerns into account.